At a spring competition, an 11 year old gymnast injured her right knee. As it was the end of the season, she was able to take the summer off and had minimal complaints all summer. Upon returning to her competitive training in September, she started to complain of pain in the same knee and she rated the pain at an 8 on a scale of 1-10. At this point, she was started natural anti-inflammatory and homeopathic remedies which included Ruta & Rhus tox homeopathics, Calc fluor tissue salt, SinewGen, Omega 3’s, hydrotherapy, castor oil packs and Traumeel cream. After an x-ray and an MRI, her pediatrician told her parents that she had a transverse fracture on the inferior patella and a torn patellar tendon. Further interpretation of the MRI estimated that 50% of her patellar tendon was torn. She was referred to a pediatric orthopedic surgeon in Edmonton who recommended rest, physiotherapy and anti-inflammatory medication for 3 months. Upon returning home to Fort McMurray and starting physiotherapy, she experienced increased swelling and pain in the knee. In addition, she felt more strain on her MCL, so her parents investigated prolotherapy as an option and scheduled a consultation to discuss their options. They also went to another Orthopedic surgeon for a third opinion.
I can relate to this patient’s case on a personal level as in 2002, I fractured my patella playing hockey. At that time, prolotherapy was not an option, and after trying many different alternative therapies, the most relief and healing I experienced was when I maintained my leg in full extension using a knee brace for two months. I also applied Symphytum salves on a daily basis to help the bone heal. As such, I advised the following:
– continue the natural anti-inflammatory protocol
– Lock the knee in full extension with a Velcro cast and not bend the leg for at least 2 weeks.
– Prolotherapy treatment
It is interesting to note that the suggestion to lock her knee was also recommended by the second orthopedic specialist. The goal of locking the leg for a short period of time (i.e. 2 weeks versus 2 months) was to prevent muscle wasting. While I locked my leg for two months, the patient was young enough that two weeks seemed sufficient. This specialist also diagnosed her with Sinding-Larsen-Johansson Syndrome. However, the pediatrician, orthopedic specialist and physiotherapist, did not agree with the recommendation of prolotherapy. Her parents contacted me and we further discussed the pros and cons of not doing the treatment and her parents felt comfortable with proceeding.
Prolotherapy is also known as “nonsurgical ligament reconstruction” and is a treatment for acute or chronic musculoskeletal pain. The word “Prolo” is short for proliferation as the treatment enhances the growth and formation of new ligaments, tendons and cartilage in areas where there is weakness or excess scar tissue. Any joint in the body can be treated successfully with Prolotherapy regardless of when the injury happened.
Prolozone combines the technique of prolotherapy using a proprietary mixture of ozone (O3) and oxygen (O2) at different strengths to stimulate blood flow to heal damaged areas. This therapy is used to treat neck pain, back pain, arthritic hips and knees, shoulder and elbow pain, degenerated disks, rotator cuff injuries and many more musculoskeletal problems. In fact, according to the official prolozone website, prolozone has a 75% success rate at completely relieving pain! 1
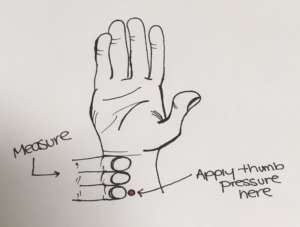
The first injection was administered to the superior and inferior poles of the right patella, including the quadriceps and patellar tendons in October. Following the treatment, the area was tender and sore which is an expected outcome. It was advised to use ice and Tylenol to control the pain. The following week, the patient’s mother reported that she was doing really well and reported her knee pain had decreased to a 1-2 out of 10 from a previously reported 8/10. The reason for the pain was now muscular due to her legs being sore from the restricted mobility the brace has provided. She was weight bearing really well and walking without the brace periodically, although she still had not bent her knee.
The second prolozone treatment was performed 3 weeks later in the same locations. Four days later, I received a message from her mother that read: “for the first time since the summer, her knee pain is finally at a 0!!!” Approximately two weeks later the physiotherapist who had performed the first knee assessment on the patient was revisited. He remarked that if he had not known the case and had not done the initial assessment himself, he would not have believed the fact that she now had a perfectly healthy knee. He could not find anything wrong on the follow up assessment, which was less than 2 months after the original prolozone treatment. The patient has returned to her gymnastics with no further complaints of knee pain.