7 Birth Control Options Besides “The Pill” by Dr. Christina Bjorndal and Lachlan Crawford
The combination oral contraceptive pill (OCP) is typically a combination of estrogen and progestin taken orally to prevent female fertility and pregnancy. It was first introduced in 1960 and since then it has undergone many modifications and has been used by millions of women  worldwide. Of Canadian women who use contraception, 32% use the OCP as their method of birth control1. It is one of the most used forms of contraception in Canada, but more and more women are looking to alternatives to oral hormonal contraceptive methods. What follows is an overview of some of the most common alternatives to “the pill”. Birth control is a personal choice and it is your right to be informed of the options available for safe and effective contraception.
worldwide. Of Canadian women who use contraception, 32% use the OCP as their method of birth control1. It is one of the most used forms of contraception in Canada, but more and more women are looking to alternatives to oral hormonal contraceptive methods. What follows is an overview of some of the most common alternatives to “the pill”. Birth control is a personal choice and it is your right to be informed of the options available for safe and effective contraception.
The Copper IUD (ParaGuard)
A copper IUD is a small medical device that is inserted into the uterus and remains there as an effective form of contraception for 5 to 12 years2. This IUD releases copper ions into the uterine cavity that interferes with sperm so that they are no longer viable to travel or to fertilize an egg, although the mechanism for this is not well understood3. Copper IUDs have become more popular in recent years because it is highly effective (only 2% of women will have unplanned pregnancies within the first year), relatively low-maintenance, and cost-effective over the long-term. It contains no hormones and is preferred by women who cannot take hormonal birth control methods. However, copper IUDs can increase cramping, pain and spotting in the first 3-6 months after it is inserted. A woman with a copper IUD will still get her period every month. In fact, the copper IUD is known to increase menstrual bleeding significantly, and has been shown to increase risk of iron-deficiency anemia. For this reason it is not recommended to women with low blood iron, ferritin or hemoglobin4. Different versions of the copper IUD are effective for varying time frames, with the ParaGuard being approved for the longest – 10 years. New studies are showing it to be effective at preventing pregnancy for up to 12 years, but should be changed at that point to ensure proper copper levels for efficacy2.
However, copper IUDs can increase cramping, pain and spotting in the first 3-6 months after it is inserted. A woman with a copper IUD will still get her period every month. In fact, the copper IUD is known to increase menstrual bleeding significantly, and has been shown to increase risk of iron-deficiency anemia. For this reason it is not recommended to women with low blood iron, ferritin or hemoglobin4. Different versions of the copper IUD are effective for varying time frames, with the ParaGuard being approved for the longest – 10 years. New studies are showing it to be effective at preventing pregnancy for up to 12 years, but should be changed at that point to ensure proper copper levels for efficacy2.
Mineral levels in the body are tightly regulated and have significant effects on body processes if levels are too high or too low. In fact, an excess of one mineral can antagonize other minerals and lead to a broader mineral imbalance. Different research groups looking at the effects of the copper IUD have found that blood levels of copper are raised to varying degrees, with newer data suggesting significant increases in serum copper5,6,7.
Copper is an essential mineral that is used in many body processes, but at excessive levels it is harmful to the body and negatively impacts the level of other essential mineral. A mineral imbalance caused by an increase in copper affects may physiological systems and can lead to hypothyroidism, emotional lability, problems with memory and concentration, poor blood glucose regulation and an increase in inflammatory conditions8. According to Julie Casper, L. Ac., and Rick Malter, Ph.D., of nutritional balancing.org, symptoms of copper excess include:
| Fatigue, exhaustion |
Headaches, migraines |
Depression |
Constipation |
PMS |
| Hypothyroidism |
Pounding heart/palpitations |
Dry skin |
Arthritis, calcium spur0s |
Aching muscles |
| Concentration and memory problems, brain fog |
Supersensitive, “over-emotional” |
Feelings of loss of control or of hopelessness |
Recurrent yeast infections |
Low blood sugar and blood pressure |
| Chocolate cravings |
Cold hands/feet |
Mood swings |
Eating disorders |
Obsessive thoughts |
“As copper increases in the body, potassium levels will be lowered and calcium levels will increase. This shift has a tendency to slow the activity of the thyroid gland. With the lowering of the potassium, the Na/K (sodium: potassium) ratio will increase, thereby putting the individual in a more chronic “fight” or “flight” response. Sodium may increase with a corresponding drop in magnesium levels. Therefore, a buildup of excess copper will tend to contribute to more intense feelings of fear and anger in a person. As more and more excess copper builds up, it will lead to a shift from anger and fear to rage and terror or panic. Such intense emotion involving rage and terror or panic will leave such a person feeling “out of control.” This is a very common reaction of a person with high copper levels.”8
Although researchers have not agreed on the possibility of copper toxicity from this contraception device, case studies are pointing to possible adverse effects, from emotional to physical9. Research on human copper toxicity remains “surprisingly sparse,” says Terry Gordon, a professor at New York University’s department of environmental medicine9. Animal studies show damage to cervical and ovarian cells from high local concentrations of copper ions from the IUD10. Perhaps the most significant study done on this topic on humans showed increased systemic biomarkers of oxidative stress and inflammation, and the authors concluded the copper IUD should be used for no more than 2 consecutive years11 as opposed to its usual recommendation of up to 5 years. New research on the etiology of psychological conditions is showing inflammation plays a significant role in the development of mental health concerns. This link shows how copper, inflammation and emotions are all connected.
In terms of mineral imbalances, serum Iron levels have been shown to decrease12 likely due to increased blood loss from heavier menstruation, as mentioned above. Serum zinc levels have actually been shown to increase with use of a copper IUD6,12, which is surprising since copper is known to be a zinc antagonist in the body – the mechanism of action of how this occurs remains unknown to researchers. On hypothesis is that serum levels of any mineral other than iron aren’t meant to be high in the blood as they are used by the body at the tissue level. As such, it would make more sense to analyze mineral deficiencies using a tissue sample (ie hair) or urine source and perhaps the research is misguided because the wrong medium is being measured.
It is important to get a good idea of what your chosen method of contraception means for your body in the short and long term. The copper IUD is growing in popularity because of its convenience, effectiveness and absence of hormones, but a broad body of research on it is still lacking. Many women have had successful and satisfactory contraception with the use of a copper IUD. It may still be a good option for you if you are sensitive to other hormonal treatments or prefer it to barrier methods, but it is important to be aware of the link between excess copper, inflammation and emotions. The best suggestion is to get your mineral levels tested by a Naturopathic doctor prior to having an IUD inserted to determine what your pre-existing levels of copper and other essential minerals are. Based on the results, an individualized mineral supplementation program can be created which will help prevent potential side effects that may result after the insertion of the copper IUD. The cost to do a hair essential mineral test is approximately $110.
The Hormonal IUD (Mirena)
The hormonal IUD, Mirena, is similar to the copper IUD in that it is a small device inserted into the uterus and remains there as long-term birth control for up to 5 years, though like the copper IUD, in some circumstances it may be used for longer. It is designed to release small amounts of a form of the female hormone progestin, like that in the oral contraceptive pill, into the uterus. While it is unclear how this inhibits female fertility, it is thought to work by thickening cervical mucus (to prevent sperm from entering the uterus and reaching or fertilizing an egg) and thinning the lining of the uterus (to make it less hospitable to egg implantation if there is fertilization)13. In the first 3-6 months after insertion, bleeding and spotting may be irregular but over time many women experience lighter and shorter menstrual bleeding than before insertion, however, some may even see a complete cessation in menstruation13.
 Mirena is 99% effective in preventing pregnancy and, like the copper IUD, is low-maintenance and cost-effective over the long term versus other methods of birth control. It does contain the hormone levonorgestrel (progestin), but because it is in the uterus the hormone levels are less than is used in the oral contraceptive pill and is effective without having systemic exposure to synthetic hormones.
Mirena is 99% effective in preventing pregnancy and, like the copper IUD, is low-maintenance and cost-effective over the long term versus other methods of birth control. It does contain the hormone levonorgestrel (progestin), but because it is in the uterus the hormone levels are less than is used in the oral contraceptive pill and is effective without having systemic exposure to synthetic hormones.
Less than 1% of women with a Mirena IUD inserted in the last year will become pregnant. However, if pregnancy does occur, it is more likely to be an ectopic pregnancy wherein implantation occurs outside the uterus. This is a potentially life-threatening concern requiring emergency care. Equally unlikely but important to know, the Mirena can also embed itself into or perforate through the lining of the uterus and migrate into the abdomen, causing serious complications requiring surgery. These risks occur in less than 1% of women who are using the Mirena IUD, but they are serious and important to calculate in your decision for birth control. The most common side effects of the Mirena are irregular bleeding (52%), headaches (12%), breast tenderness (3-9%), acne (15%), inflammation of the vulva/vagina (20%), development of ovarian cysts (13%), loss of periods (1-12%), mood changes (4%), and pelvic pain (12%)14. New studies are claiming that it is effective at preventing pregnancy even up to one year after its FDA-approved time of 5 years, though this may result in more difficulty conceiving after its removal15. Use beyond 6 years is not recommended as it may be ineffective and lead to unwanted pregnancy.
As there is a chance you may stop your period altogether while using the Mirena, it is a good idea to decide if you feel comfortable with this possibility. Although the Society of Obstetricians and Gynecologists of Canada (SOGC) and the Association of Reproductive Health Professionals (ARHP) state there is no evidence that suppression of periods is harmful, it is important to note that there are no long-term studies to specifically investigate this16,17. Menstruation, contraception and fertility are deeply intimate topics that have been debated by politics and religion for generations. As a result they can hold cultural significance in addition to their biological purpose. Fortunately women now have the ability to choose the significance for themselves and make that a biological reality. For an in-depth discussion of the history, pros and cons of missing periods, please read the article “A Brief History of your Period and Why you don’t have it” by Psychologist Valerie Tarico in the feminist magazine Jezebel.
“The Ring” and “The Patch”
The ring and the patch are two variations on the combined oral contraceptive pill and therefore have much the same risks, side effects and contraindications as “the pill”18. Products such as the NuvaRing and Evrapatch deliver female hormones (both estrogen and progestin) for three weeks to block ovulation and prevent pregnancy18. 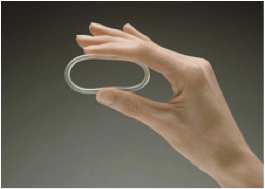 The ring is inserted into the vagina whereas the patch is placed on the skin. After three weeks of hormone delivery, the ring or skin patch is removed and allows for a withdrawal bleed that imitates a period, like the oral contraceptive pill. These methods work differently than the Mirena because the method of action is to block ovulation and does not necessarily modify the cervical mucus or uterine lining.
The ring is inserted into the vagina whereas the patch is placed on the skin. After three weeks of hormone delivery, the ring or skin patch is removed and allows for a withdrawal bleed that imitates a period, like the oral contraceptive pill. These methods work differently than the Mirena because the method of action is to block ovulation and does not necessarily modify the cervical mucus or uterine lining. 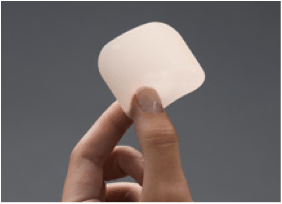 With perfect use, both the ring and the patch are 99.7% effective at preventing pregnancy and with typical use, 92%19.
With perfect use, both the ring and the patch are 99.7% effective at preventing pregnancy and with typical use, 92%19.
The Diaphragm
This is a barrier method that involves no hormones and no future impact on fertility. The diaphragm is a flexible latex or silicone dome-shaped device filled with spermicide and inserted into the upper vagina covering the cervix. It creates a spermicidal barrier at the cervical opening and must be used with the spermicidal gel to be effective. Women can insert the diaphragm up to 6 hours before intercourse and should leave it in place for at least 6 hours after (up to 24 hrs)18. If there is more than one occurrence of intercourse in the 24 hours without removal, more spermicidal gel can be added to be sure.
Used correctly and consistently, the diaphragm is 94% effective at preventing pregnancy, though with typical use is 84%. For full effectiveness, the diaphragm does require active participation from the woman: proper hygiene habits and regular insertion, cleaning, removal and storage. Using a diaphragm may increase the incidence of urinary tract infections due to the manual insertion and removal. In the past, it needed to be fitted by a physician as well to ensure comfort and effectiveness.
Up to 25% of married women in 1955 were using the diaphragm19, but when the birth control pill was introduced and women had the option to have contraception with much less maintenance, the popularity of the diaphragm dropped dramatically.  According to the Canadian National Contraception Survey in 2009, only 0.2% of women using contraception choose the diaphragm21.
According to the Canadian National Contraception Survey in 2009, only 0.2% of women using contraception choose the diaphragm21.
Due to its lowered popularity, there has been limited access to the diaphragm in Canada in recent decades. However, more women are now looking for alternatives to hormonal treatment and the diaphragm is seeing resurgence. New diaphragm products are coming onto the market that are designed to manage some of the drawbacks to the old designs. A new product called Caya, for example, is designed to fit most women and eliminates the need for fitting by a physician. The advantages remain the same as other barrier methods: no hormonal modification or changes to fertility of either party, and the disadvantages are relative to other methods available; the diaphragm requires more active participation from the woman but with proper use is just as effective as using male condoms19.
Male condoms, with and without spermicide
The use of male condoms is one of the most common methods of birth control. With perfect use it is 98% effective at preventing pregnancy, though this rate drops to 85% with typical use19. Perfect use means applying the condom before any sexual contact, being sure that it does not slip or tear, and removing it immediately after male ejaculation – and this must be done consistently and correctly every single time. Therefore, technique and consistency is key for this method – it requires commitment from both you and your partner to ensure you are both as protected as possible.
 Using additional spermicidal gel or foam can increase the effectiveness of this method, though it’s not confirmed exactly how effective typical use with extra spermicidal protection is. The advantage of condoms is that it is hormone-free and also very effective at protecting against sexually transmitted infections and HIV. It is a lifestyle choice that requires engagement from the male partner and can offer opportunity to talk about sexuality, safety and concerns with each other. Note that it is important not to use latex-based lube with latex condoms or to use two condoms at once as both of these may increase the risk of breakage19.
Using additional spermicidal gel or foam can increase the effectiveness of this method, though it’s not confirmed exactly how effective typical use with extra spermicidal protection is. The advantage of condoms is that it is hormone-free and also very effective at protecting against sexually transmitted infections and HIV. It is a lifestyle choice that requires engagement from the male partner and can offer opportunity to talk about sexuality, safety and concerns with each other. Note that it is important not to use latex-based lube with latex condoms or to use two condoms at once as both of these may increase the risk of breakage19.
Fertility Awareness Method (Rhythm Method)
Fertility Awareness is a way to predict your body’s fertile and infertile times during your cycle. Based on the knowledge that the body shows visible and detectable signs of hormonal changes throughout the cycle, a female can know the date of ovulation, and therefore, know when they are fertile and when they are not. During the fertile periods during the cycle, one must abstain completely from sex or use another effective method to prevent pregnancy. This is a wonderful way to get to know your body as you track cycles and get in touch with what is happening and when. It can be extremely effective if you are diligent and consistent. With theoretical perfect use (meaning you are very good at knowing exactly when you ovulate) it is 95-97% effective. However because this method requires consistent and careful monitoring, typical use falls to about 75%19.
 The fertility awareness method is based on the fact that an egg is released once in each menstrual cycle, usually around mid-cycle, and can live for 12 to 24 hours, waiting to be fertilized before menses flushes out the egg and the uterine lining. Sperm can live in the female reproductive tract up to 6 days and fertilize an egg. Therefore, a female is fertile for as long as six days before ovulation and two or three days after ovulation, a total of seven to eight days of fertility in her cycle each month22. During these fertile days, other contraceptive methods must be used, and outside these days, she is considered infertile and unable to become pregnant. Of course, this method does not protect against sexually transmitted infections.
The fertility awareness method is based on the fact that an egg is released once in each menstrual cycle, usually around mid-cycle, and can live for 12 to 24 hours, waiting to be fertilized before menses flushes out the egg and the uterine lining. Sperm can live in the female reproductive tract up to 6 days and fertilize an egg. Therefore, a female is fertile for as long as six days before ovulation and two or three days after ovulation, a total of seven to eight days of fertility in her cycle each month22. During these fertile days, other contraceptive methods must be used, and outside these days, she is considered infertile and unable to become pregnant. Of course, this method does not protect against sexually transmitted infections.
There are different approaches to detecting ovulation that are available to learn, including using a calendar to track cycles, assessing cervical mucous thickness, checking basal body temperature daily, and breast tenderness22. Keep in mind that your cycle itself can vary depending on many factors such as stress, change, trauma, illness and allergic reactions, making it sometimes difficult to be certain of timing. If you are interested in the fertility awareness method, be sure that both you are your partner(s) are committed and there is consistency in the tracking. If done properly this is a natural and effective way to prevent pregnancy.
Making an Informed Decision
Birth control is an important and intimate decision. If you are looking for alternatives to the oral contraceptive pill, know there are options available for you. Your body does not have to follow any method but what is right for you. Talk with your health care provider about your options, be informed of all the effects of each method and determine what is safe and comfortable for you at this time in your life.
Relative Effectiveness of Birth Control Methods at Preventing Pregnancy19
| Method used |
EffectivenessPERFECT USE |
EffectivenessTYPICAL USE |
| OCP/The Pill |
99.7% |
92% |
| The Patch |
99.7% |
92% |
| The Ring |
99.7% |
92% |
| Hormonal IUD, Mirena |
99.9% |
99.9% |
| Copper IUD, ParaGuard |
99.4% |
99.2% |
| Diaphragm with spermicide |
94% |
84% |
| Male Condoms + spermicide |
99% |
No confirmed data |
| Male condoms alone (no spermicide) |
98% |
85% |
| Fertility Awareness Method |
97-95% |
75% |
| Withdrawal (pulling out) |
96% |
73% |
| No birth control |
15% |
15% |
References
All photos used are under a Creative Commons Attribution-Non Commercial-NoDerivs License from the Association of Reproductive Health Professionals at http://www.arhp.org/
- Society of Obstetricians and Gynecologists of Canada, Canadian Contraception Consensus, SOGC Clinical Practice Guidelines, 2004. http://sogc.org/wp-content/uploads/2013/01/143E-CPG2-March2004.pdf
- Doyle, K., 2014. IUD Effective for Longer than Recommended. Reuters Health News. http://www.reuters.com/article/us-iuds-effective-idUSBREA2C1B320140313
- Island Sexual Health, Copper IUD, Beyond the Talk.ca http://beyondthetalk.ca/birth-control-pregnancy/birth-control/ec/copper-iud/
- Andrade et. al., 1987. Quantitative studies on menstrual blood loss in IUD users Jul;36(1):129-44. http://www.ncbi.nlm.nih.gov/pubmed/3311622
- Prema et. al.,1980. Serum copper in long-term users of copper intrauterine devices. Fertil Steril.Jul;34(1):32-5 http://www.ncbi.nlm.nih.gov/pubmed/7398904
- Imani et. al, 2014. Changes in copper and zinc serum levels in women wearing a copper TCu-380A intrauterine device. Eur J Contracept Reprod Health Care. Feb;19(1):45-50 http://www.ncbi.nlm.nih.gov/pubmed/24304153
- De la cruz et. al., 2005. Blood copper levels in Mexican users of the T380A IUD. Contraception, Vol.72; Issue 2, Pgs. 122–125 http://www.contraceptionjournal.org/article/S0010-7824(05)00075-2/abstract
- Julie Casper and Rick Malter for Nutr.balancing.org, 2016. Copper Toxicity.http://nutritionalbalancing.org/center/htma/science/articles/copper-toxicity.php
- Scilla Alecci for Women’s News, 2015. In Online Forums, Women Share Copper IUD Fearshttp://womensenews.org/2015/03/in-online-forums-women-share-copper-iud-fears/
- Grillo et. al., 2010. Does over-exposure to copper ions released from metallic copper induce cytotoxic and genotoxic effects on mammalian cells? Vol.81;Issue 4, Pgs 343–349 http://www.contraceptionjournal.org/article/S0010-7824(09)00521-6/abstract
- Arnal et al., 2010. Alterations in copper homeostasis and oxidative stress biomarkers in women using the intrauterine device TCu380A. Toxicology Letters. Vol.192;Issue 3, Pgs 373-378 http://www.sciencedirect.com/science/article/pii/S0378427409015264
- Fahmy et. al., 1993. Serum and endometrial copper, zinc, iron and cobalt with inert and copper-containing IUCDs.May;47(5):483-90. http://www.ncbi.nlm.nih.gov/pubmed/8513675
- Official Mirena website, 2016. Bayer Pharmaceutical Company. http://www.mirena-us.com/about-mirena/how-mirena-works.php
- Medscape 2016. Levonorgestrel intrauterine (Rx) Adverse Effects. http://reference.medscape.com/drug/mirena-skyla-levonorgestrel-intrauterine-342780#4
- Lawson, A., 2015. Research Shows IUDs May Prevent Pregnancy Longer Than Expected. Surgical Watch.http://surgicalwatch.com/2015/02/research-shows-iuds-prevent-pregnancy-longer-expected/
- McQuillan et. al., 2013. Menstrual Suppression in Special Circumstances. Clinical Guidelines for the Society of Obstetricians and Gynecologists of Canada. http://sogc.org/guidelines/menstrual-suppression-special-circumstances/
- Kaunitz et. la., 20018.. Understanding Menstrual Suppression. Association of Reproductive Health Professionals (ARHP) http://www.arhp.org/uploadDocs/understandingmenstrualsuppression.pdf
- Association of Reproductive Health Professionals (ARHP) , 2014. Choosing a Birth Control Method.http://www.arhp.org/Publications-and-Resources/Quick-Reference-Guide-for-Clinicians/choosing
- Options for Sexual Health, 2009. Relative Effectiveness of Birth Control Methodshttps://www.optionsforsexualhealth.org/birth-control-pregnancy/birth-control-options/effectiveness
- CDC, 2002. Use of Contraception and Use of Family Planning Services in the United States: 1982-2002.http://www.cdc.gov/nchs/data/ad/ad350FactSheet.pdf
- Black et.al., 2009. Contraceptive Use Among Canadian Women of Reproductive Age: Results of a National Survey. J Obstet Gynaecol Can. Jul;31(7):627-40. http://www.sexualityandu.ca/uploads/files/National_Contraception_Survey.pdf
- Options for Sexual Health. 2009. Fertility Awareness Method. https://www.optionsforsexualhealth.org/birth-control-pregnancy/birth-control-options/natural-methods/fam

 I go on to explain that I understand how difficult it is when you are in the pit of depression & despair to exercise. I also share that there have been times that THAT is all that I have “accomplished” in a day. The struggle to get myself out the door has been agony at times. It has taken me several hours – 2, 4, 6, 8 or 10 hours at times – to move from my bedroom to the door. When I am depressed, the battle between the side of me that wants to get well and the side of me that is stuck in depression and defeat can be paralyzing and it can take hours to muster up the courage to do all the steps required to get me out the door:
I go on to explain that I understand how difficult it is when you are in the pit of depression & despair to exercise. I also share that there have been times that THAT is all that I have “accomplished” in a day. The struggle to get myself out the door has been agony at times. It has taken me several hours – 2, 4, 6, 8 or 10 hours at times – to move from my bedroom to the door. When I am depressed, the battle between the side of me that wants to get well and the side of me that is stuck in depression and defeat can be paralyzing and it can take hours to muster up the courage to do all the steps required to get me out the door: I credit tennis to lifting a depression that had been weighing me down for several months in 2008. A friend asked me to play and we started playing a few nights a week. I was now engaging in a social activity with a friend, getting outside in the fresh air, getting sunlight/Vit D and was stimulating my appetite because of the exercise. After 2 months of this, I was no longer depressed!
I credit tennis to lifting a depression that had been weighing me down for several months in 2008. A friend asked me to play and we started playing a few nights a week. I was now engaging in a social activity with a friend, getting outside in the fresh air, getting sunlight/Vit D and was stimulating my appetite because of the exercise. After 2 months of this, I was no longer depressed! worldwide. Of Canadian women who use contraception, 32% use the OCP as their method of birth control1. It is one of the most used forms of contraception in Canada, but more and more women are looking to alternatives to oral hormonal contraceptive methods. What follows is an overview of some of the most common alternatives to “the pill”. Birth control is a personal choice and it is your right to be informed of the options available for safe and effective contraception.
worldwide. Of Canadian women who use contraception, 32% use the OCP as their method of birth control1. It is one of the most used forms of contraception in Canada, but more and more women are looking to alternatives to oral hormonal contraceptive methods. What follows is an overview of some of the most common alternatives to “the pill”. Birth control is a personal choice and it is your right to be informed of the options available for safe and effective contraception. However, copper IUDs can increase cramping, pain and spotting in the first 3-6 months after it is inserted. A woman with a copper IUD will still get her period every month. In fact, the copper IUD is known to increase menstrual bleeding significantly, and has been shown to increase risk of iron-deficiency anemia. For this reason it is not recommended to women with low blood iron, ferritin or hemoglobin4. Different versions of the copper IUD are effective for varying time frames, with the ParaGuard being approved for the longest – 10 years. New studies are showing it to be effective at preventing pregnancy for up to 12 years, but should be changed at that point to ensure proper copper levels for efficacy2.
However, copper IUDs can increase cramping, pain and spotting in the first 3-6 months after it is inserted. A woman with a copper IUD will still get her period every month. In fact, the copper IUD is known to increase menstrual bleeding significantly, and has been shown to increase risk of iron-deficiency anemia. For this reason it is not recommended to women with low blood iron, ferritin or hemoglobin4. Different versions of the copper IUD are effective for varying time frames, with the ParaGuard being approved for the longest – 10 years. New studies are showing it to be effective at preventing pregnancy for up to 12 years, but should be changed at that point to ensure proper copper levels for efficacy2. Mirena is 99% effective in preventing pregnancy and, like the copper IUD, is low-maintenance and cost-effective over the long term versus other methods of birth control. It does contain the hormone levonorgestrel (progestin), but because it is in the uterus the hormone levels are less than is used in the oral contraceptive pill and is effective without having systemic exposure to synthetic hormones.
Mirena is 99% effective in preventing pregnancy and, like the copper IUD, is low-maintenance and cost-effective over the long term versus other methods of birth control. It does contain the hormone levonorgestrel (progestin), but because it is in the uterus the hormone levels are less than is used in the oral contraceptive pill and is effective without having systemic exposure to synthetic hormones.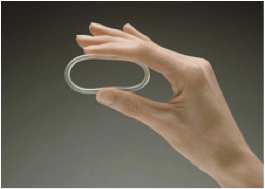 The ring is inserted into the vagina whereas the patch is placed on the skin. After three weeks of hormone delivery, the ring or skin patch is removed and allows for a withdrawal bleed that imitates a period, like the oral contraceptive pill. These methods work differently than the Mirena because the method of action is to block ovulation and does not necessarily modify the cervical mucus or uterine lining.
The ring is inserted into the vagina whereas the patch is placed on the skin. After three weeks of hormone delivery, the ring or skin patch is removed and allows for a withdrawal bleed that imitates a period, like the oral contraceptive pill. These methods work differently than the Mirena because the method of action is to block ovulation and does not necessarily modify the cervical mucus or uterine lining. 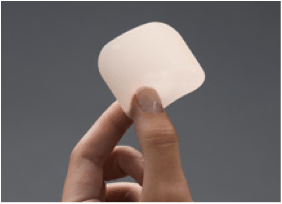 With perfect use, both the ring and the patch are 99.7% effective at preventing pregnancy and with typical use, 92%19.
With perfect use, both the ring and the patch are 99.7% effective at preventing pregnancy and with typical use, 92%19. According to the Canadian National Contraception Survey in 2009, only 0.2% of women using contraception choose the diaphragm21.
According to the Canadian National Contraception Survey in 2009, only 0.2% of women using contraception choose the diaphragm21. Using additional spermicidal gel or foam can increase the effectiveness of this method, though it’s not confirmed exactly how effective typical use with extra spermicidal protection is. The advantage of condoms is that it is hormone-free and also very effective at protecting against sexually transmitted infections and HIV. It is a lifestyle choice that requires engagement from the male partner and can offer opportunity to talk about sexuality, safety and concerns with each other. Note that it is important not to use latex-based lube with latex condoms or to use two condoms at once as both of these may increase the risk of breakage19.
Using additional spermicidal gel or foam can increase the effectiveness of this method, though it’s not confirmed exactly how effective typical use with extra spermicidal protection is. The advantage of condoms is that it is hormone-free and also very effective at protecting against sexually transmitted infections and HIV. It is a lifestyle choice that requires engagement from the male partner and can offer opportunity to talk about sexuality, safety and concerns with each other. Note that it is important not to use latex-based lube with latex condoms or to use two condoms at once as both of these may increase the risk of breakage19.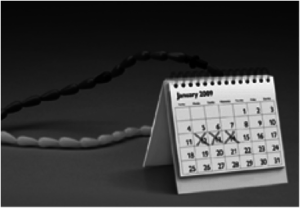 The fertility awareness method is based on the fact that an egg is released once in each menstrual cycle, usually around mid-cycle, and can live for 12 to 24 hours, waiting to be fertilized before menses flushes out the egg and the uterine lining. Sperm can live in the female reproductive tract up to 6 days and fertilize an egg. Therefore, a female is fertile for as long as six days before ovulation and two or three days after ovulation, a total of seven to eight days of fertility in her cycle each month22. During these fertile days, other contraceptive methods must be used, and outside these days, she is considered infertile and unable to become pregnant. Of course, this method does not protect against sexually transmitted infections.
The fertility awareness method is based on the fact that an egg is released once in each menstrual cycle, usually around mid-cycle, and can live for 12 to 24 hours, waiting to be fertilized before menses flushes out the egg and the uterine lining. Sperm can live in the female reproductive tract up to 6 days and fertilize an egg. Therefore, a female is fertile for as long as six days before ovulation and two or three days after ovulation, a total of seven to eight days of fertility in her cycle each month22. During these fertile days, other contraceptive methods must be used, and outside these days, she is considered infertile and unable to become pregnant. Of course, this method does not protect against sexually transmitted infections.